Mpox Outbreak In The EU Explained: Key Facts, Insights, And Preventive Measures
Key Points On The Mpox Outbreak
- Mpox, or monkeypox, is a disease caused by a virus similar to smallpox. It mostly happens in parts of Africa, but recently, it has spread to other places in the world. People with Mpox usually get flu-like symptoms such as fever, chills, and a rash that can last a few weeks.
- The virus can spread from one person to another through close contact, such as touching someone with the rash or through clothes or bedding the infected person has used. It can also spread from animals to humans.
- In 2024, a new and more dangerous strain of Mpox, known as Clade IIb, has been spreading in Europe, Africa, and other parts of the world. The World Health Organization (WHO) has declared it a global health emergency, which means the world needs to take it seriously.
- Experts say Mpox differs from Covid-19 because we know better ways to control it. Vaccines originally made for smallpox also work against Mpox, and people who are at risk are being vaccinated. Health officials are also keeping a close watch on new cases.
- The best way to avoid getting Mpox is to stay away from people who have it and avoid touching things they’ve used. Vaccination can help protect people who are more likely to get the virus.
- In 2024, almost 14000+ cases of Mpox have been reported, with nearly 524 deaths. This number is enormous compared to the last year’s stats.
Mpox Overview:
Mpox, previously called monkeypox, is a disease caused by a virus in the same family as smallpox. It leads to symptoms like fever, headaches, muscle aches, swollen lymph nodes, and a rash that starts as flat spots and then turns into blisters. Most people recover in 2-4 weeks. Still, some groups, like children, pregnant people, and those with weakened immune systems, can get seriously ill.
The virus was first discovered in monkeys in 1958 in Denmark, where it got its name. The first human case was reported in 1970 in the Democratic Republic of the Congo (DRC). Mpox has mainly affected African countries for many years. Still, in 2022, the virus started spreading to other parts of the world, including Europe and US.
The virus spreads mainly through close contact with an infected person, such as touching their skin, sharing bedding, or breathing in respiratory droplets. You can also catch it by handling animals carrying the virus or touching contaminated items like clothing. Mpox is most common in parts of Africa. Still, recent outbreaks have happened in other regions, including the U.S. and Europe. The 2022-2023 global outbreak was mainly caused by a variant of the Clade IIb virus.
To prevent Mpox, vaccines like Jynneos are available and recommended for people at higher risk, such as healthcare workers or those with known exposure to the virus. Vaccination can help reduce the severity of the disease. Even though cases have risen in some areas, experts say the outbreak is not as widespread as other recent pandemics, like COVID-19. With ongoing vaccinations and careful public health measures, the spread of Mpox can be controlled.
How is Mpox Transmitted?
The Mpox can be transmitted in several ways. The main transmission mediums of Mpox are:
1. Person-to-person transmission
- Direct contact with infectious skin lesions, such as those on the mouth, genitals, or other body parts.
- Face-to-face contact that involves respiratory droplets and close interaction for a long time.
- Having physical contact with an infected person, such as touching, kissing, performing sexual activities, and more.
- Contact with contaminated materials like clothing, bedding, towels, or other objects.
2. Animal To Human Transmission
- Getting bites or scratches from infected animals.
- Performing activities like hunting, cooking, or skinning of infected animals.
- Consuming meat of an infected animal that hasn’t been cooked properly and handling animal products like fur.
3. Object To Human Transmission
- Touching infected objects like surfaces, clothing, tools, linens, etc.
- Having sharp injuries from infected objects in healthcare settings, tattoo parlours, etc.
What Are The Signs And Symptoms of Mpox
Mpox, or monkeypox, usually starts with flu-like symptoms and a rash. Symptoms typically show up one to 21 days after exposure to the virus. Once they start, symptoms typically last two to four weeks, but for people with weaker immune systems, they could last longer.
Here’s what to look out for:
- Fever
- Headache
- Muscle aches
- Back pain
- Sore throat
- Low energy
- Swollen lymph nodes (These are small, bean-shaped glands that might feel sore or lumpy under your skin, especially around your neck or groin.)
One of the most noticeable symptoms of Mpox is a rash. This rash starts as flat red spots that eventually become liquid blisters. These blisters can hurt or itch. Over time, they become pus-filled bumps, scab over, and eventually fall off as the skin heals. The rash can show up almost anywhere on your body, like your face, mouth, hands, feet, and even private areas like the groin or anus.
Some people get many of these bumps, while others may only have a few. In some cases, the rash is the first thing you’ll notice, while in others, flu-like symptoms like fever, headache, and muscle aches come first. Some people may not even get a rash or only have mild symptoms, but they can still spread the virus to others through close physical contact.
Mpox can also cause other problems, like painful swelling in the rectum, trouble peeing, or skin infections if the blisters worsen. Serious issues, like pneumonia, eye infections that could affect your vision, brain swelling, and heart inflammation, can also happen, especially in people with weaker immune systems.
During the 2022-2023 outbreak, a different version of the virus (called clade IIb) sometimes caused the rash to appear in unusual places, like the groin or mouth, before spreading elsewhere. The good news is that most people recover fully, but it’s important to be aware of the symptoms and seek help if needed.
If you or someone you know has pox, avoiding close contact with others is crucial until the rash has completely healed and new skin has formed over the sores.
Mpox Diagnosis
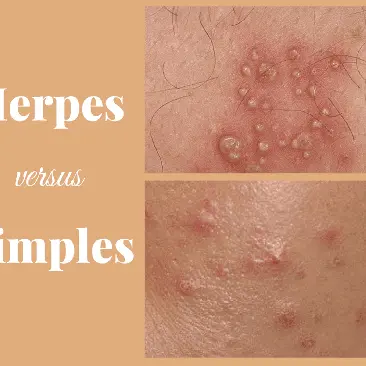
Diagnosing Mpox can be challenging because it looks like other illnesses that cause rashes, like chickenpox, measles, or skin infections. Doctors need to figure out if it's Mpox or something else, like herpes or syphilis, which can also cause similar symptoms. Sometimes, a person might simultaneously have Mpox and another infection, making it harder to tell what's happening. This is why testing is essential to get the proper treatment and stop the virus from spreading.
The best way to know if someone has Mpox is through a lab test called PCR (polymerase chain reaction). This test looks for the virus’s DNA in samples taken from the rash. Doctors usually swab the rash or the fluid from blisters to collect the sample. If there’s no rash, they might use a swab from other areas, like the throat or rectum, to test for the virus. Testing blood doesn’t help diagnose Mpox because it doesn’t give accurate results for this virus. Also, antibody tests can’t tell the difference between Mpox and other similar viruses like smallpox.
Getting tested quickly helps people with Mpox get treated sooner and prevents the virus from spreading to others.
Mpox Management and Treatment
Mpox usually gets better independently, with symptoms lasting about two to four weeks. After you’re diagnosed, your doctor will help manage your symptoms, ensure you stay hydrated, and give you antibiotics if you develop bacterial infections.
While there aren't any specific antiviral treatments for Mpox, doctors may use antiviral medications like tecovirimat or cidofovir if you get sick. These medicines were originally made to treat smallpox, but doctors are still studying how well they work for Mpox.
The main goals of treatment are to treat the rash, manage pain, and prevent complications. Early help can make a big difference in your feelings and avoid further problems.
Vaccination is another way to prevent Mpox. If you’ve been exposed to the virus, getting the vaccine within four days is best. It can still help up to 14 days after exposure if you haven't shown symptoms. Vaccines are especially recommended for people at higher risk, such as healthcare workers, men who have sex with men, people with multiple sex partners, and sex workers.
If someone has Mpox, they should stay away from others to avoid spreading the virus. Researchers continue to study the best ways to treat and manage Mpox, and more information is available during outbreaks.
How To Prevent Mpox
Preventing Mpox involves stopping the spread of the virus. Vaccination and other safety measures are key to protecting yourself and others from infection.
Mpox Vaccines
Vaccines originally developed for smallpox are also effective against Mpox. These vaccines are recommended for people exposed to Mpox or at higher risk of exposure. You might be at higher risk if:
- You’ve had close contact with someone diagnosed with Mpox.
- A recent sexual partner has been diagnosed with Mpox.
- You’ve visited places like sex clubs, bathhouses, or other venues where Mpox has been reported.
- You have multiple sexual partners.
Vaccination is most effective if received within four days of exposure. However, it can still help up to 14 days after exposure if no symptoms have appeared. Talk to a healthcare provider if you're unsure whether you should get vaccinated. If that's a concern, they can also give you the vaccine in a less visible area of your body, like the shoulder blade.
Other Prevention Methods
In addition to vaccination, there are several other ways to prevent the spread of Mpox:
- Avoid contact with infected animals, especially sick or dead animals.
- Steer clear of contaminated materials like bedding or clothing used by someone with Mpox.
- Cook animal products thoroughly before consuming them.
- Wash your hands regularly with soap and water, or use hand sanitiser.
- Avoid close contact with people who may have Mpox.
- Practice safe sex, including using condoms and dental dams.
- Wear a mask to cover your nose and mouth when around others.
- Clean and disinfect surfaces that are frequently touched.
- Use personal protective equipment (PPE) when caring for someone with Mpox.
Self-Care and Isolation
If you have Mpox, most people recover within two to four weeks. Here are some tips for managing your symptoms and preventing the virus from spreading:
- Stay home and, if possible, stay in your room.
- Wash your hands often, especially after touching sores.
- Wear a mask and cover sores when you are around other people.
- Keep your skin dry and uncovered unless you are in a shared space with others.
- Avoid touching items in shared spaces and disinfect these areas frequently.
- Rinse mouth sores with salt water and take warm baths with baking soda or Epsom salts for body sores.
- Use over-the-counter pain relievers like acetaminophen or ibuprofen for pain management.
Avoid:
- Popping blisters or scratching sores which can slow healing, spread the rash, and cause infections.
- Shaving over sores until they’ve fully healed prevents the rash from spreading.
Living With Mpox
If you have Mpox, there are things you can do to feel better and prevent spreading it to others:
- Use pain relievers and fever reducers. Medicines like ibuprofen (Advil®, Motrin®) and acetaminophen (Tylenol®) can help lower your fever and reduce pain.
- Take oatmeal baths. A warm bath with oatmeal can help soothe your skin and relieve the itching caused by the rash.
- Stay away from others. If you're infected, it's important to isolate yourself until all your sores have scabbed over and healed.
- Cover your sores with gauze or bandages to prevent the virus from spreading to other people and surfaces.
- Rest and stay hydrated. Make sure to rest, drink plenty of fluids, and wear a mask if you need to be around others.
- Avoid contact with pets. Stay away from pets, especially rodents, until you're better.
Taking care of yourself and avoiding contact with others can help you recover and keep the virus from spreading.
Mpox Across Europe
Mpox has affected countries across Europe in varying ways. This overview provides a snapshot of how different nations manage the virus and each region's current conditions.
Mpox Outbreak in France
In France, the government is taking serious steps to deal with Mpox (monkeypox). The country has put its health system on "maximum alert" to respond quickly and control the virus. The first case of Mpox in France was reported on May 20, 2022. Since the beginning of 2024, 12 to 26 new cases of Mpox reported each month.
The government is spending a lot of money on vaccines to stop the virus from spreading. They are making sure people who are at risk get vaccinated to protect themselves and others. France also runs public health campaigns to teach people how to prevent the virus and recognise the symptoms. France is working hard to manage Mpox and keep the population safe by focusing on vaccinations and public awareness.
Mpox Outbreak in Spain
Spain has recorded the highest number of Mpox (monkeypox) infections in Europe. According to the latest data from the National Ministry of Health, released on August 8, there have been 8,104 Mpox cases since the first outbreak in April 2022. However, new cases decreased significantly in 2024, with only 251 cases reported this year.
All of the Mpox infections recorded in 2024 were caused by the original strain of the virus, with no new variants emerging. The Spanish government monitors the situation closely and has implemented public health measures to prevent further spread. With ongoing vaccination efforts and public awareness campaigns, Spain is working to keep the virus under control and protect its population from future outbreaks.
Mpox Outbreak in Portugal
Between June 1, 2023, and the end of July 2024, Portugal reported 244 Mpox (monkeypox) cases, with only three occurring after May. Fortunately, none of these cases have resulted in death. The Clade IIb variant of the virus caused all the cases.
The Clade IIb variant is different from Clade I because it spreads through close contact but not necessarily through sexual contact, which makes it easier to catch. Health authorities in Portugal continue to monitor the situation closely and take steps to manage the spread of the virus. Public health efforts focus on educating people about the symptoms and encouraging preventive actions to stop further outbreaks.
Mpox Outbreak in Germany
According to the Robert Koch Institute (RKI), as of August 15, 2024, Germany reported 86 cases of monkeypox, with Berlin having the most cases out of all the German states. While pox is still present, the number of cases is much lower compared to 2022, when the virus spread more widely. By mid-August 2022, Berlin alone had over 1,500 confirmed cases.
Berlin's health administration, led by Health Senator Ina Czyborra, is keeping a close eye on the situation and is ready to take action if needed. Reflecting on the 2022 outbreak, Czyborra explained that Berlin responded well by quickly making vaccines available. Thankfully, these vaccines are now offered through the regular healthcare system, so there's no need for a special vaccination campaign this year. Authorities remain alert to ensure the virus stays controlled and the public stays safe.
Mpox Outbreak in Italy
Italy was one of the first European countries to experience a Mpox outbreak in 2022, with the first case reported in Rome on May 19, 2022. Since then, the virus has continued to circulate. In 2024, Italy reported 47 Mpox cases, a significant number occurring in Lombardy. Between October 2023 and January 2024, Lombardy recorded 44 cases, primarily among men who have sex with men (MSM). The Italian health authorities remain vigilant, focusing on vaccination and monitoring to prevent further outbreaks.
Mpox Outbreak in Ireland
In 2024, Ireland reported six Mpox (monkeypox) cases, continuing the downward trend after the global outbreak began in 2022. 2023, Ireland confirmed 13 cases, significantly lower than the 227 cases reported in 2022. The Mpox cases in 2024 have been linked to the Clade II variant responsible for the global outbreak. This strain primarily affects gays, bisexuals, and other men who have sex with men. Irish health authorities closely monitor the situation to manage and prevent further spread.
Mpox Outbreak in Austria
In 2024, Austria continued to report Mpox cases following the global outbreak that began in 2022. While the number of new cases has decreased compared to the outbreak's peak, Austria remains vigilant. The country reported 327 cases by the end of 2023, with health authorities maintaining strict monitoring and preventive measures. In 2024, there have been fewer cases, mainly due to increased vaccination efforts and public health campaigns. Austria has focused on containing the virus by ensuring vaccine access and promoting awareness of the symptoms and prevention methods. The government has also implemented guidelines to manage the outbreak, including quarantine protocols for infected individuals.
Mpox Outbreak in Switzerland
In 2024, Switzerland remains cautious about Mpox (monkeypox) following the first cases reported in May 2022. Health authorities have proactively monitored the virus through testing and prevention strategies. As of the latest reports, the country has confirmed 416 Mpox cases. The Geneva University Hospitals (HUG) played a key role by sequencing the virus from the first cases, helping researchers understand how it spreads. Vaccination is available for those at risk, and the responsibility for organising vaccinations lies with the individual cantons. People are encouraged to consult healthcare professionals to assess their risk and decide if they should be vaccinated.
Mpox Outbreak in the Netherlands
As of August 16, 2024, there have been no reported infections involving the new Mpox variant in the Netherlands. Healthcare providers nationwide remain vigilant for any symptoms of Mpox to ensure that potential infections are identified swiftly. In the event of a confirmed case, the Municipal Public Health Services (GGDs) will immediately conduct source and contact tracing to help prevent further spread. They will also guide those exposed. Close contacts of confirmed cases may receive vaccinations as a preventive measure. The Netherlands has an adequate stockpile of vaccines, ensuring they are available if needed. An antiviral medication is also available to treat any complications that may arise from an Mpox infection. This proactive approach ensures the country is prepared to manage and contain the virus effectively.
Mpox Outbreak in Malta
As of the most recent reports from health authorities in Valletta, Malta has not recorded any new Mpox (monkeypox) cases or deaths. Since the start of the global outbreak, the country has experienced 34 confirmed cases. Despite no recent rise in infections, health officials remain vigilant, monitoring the situation closely to prevent any resurgence of the virus. Preventive measures and public health initiatives are in place to ensure the population's safety. Malta's response has helped keep the spread of Mpox under control, with no new cases reported in recent months.
When To See A Doctor
Call your doctor if you:
- Feel sick with a fever, body aches, or swollen glands (lymph nodes).
- Notice a new rash or sores on your skin.
- Have been in close contact with someone who has Mpox.
Go to the ER if you have:
- Trouble breathing.
- Chest pain that starts or gets worse.
- A stiff neck.
- Confusion or trouble thinking clearly.
- Difficulty speaking or moving.
- Fainting or losing consciousness.
- Seizures (uncontrolled shaking or convulsions).
- If you notice any severe symptoms, get medical help immediately.
If you're concerned about Mpox, Mobi Doctor is here to help. You can consult healthcare professionals online for guidance on symptoms, prevention, and treatment options, all from the comfort of your home.