Mpox (Monkeypox) in 2025: Signs, Treatment & Telemedical Care in the EU
In an era where news spreads in seconds and health risks can cross continents, staying informed has never been more important. As the world continues to face emerging infectious diseases, one name that remains on the radar in 2025 is Mpox (formerly known as monkeypox). But are you prepared to navigate these evolving health challenges with clarity and confidence?
This guide cuts through the noise, offering the latest, evidence-based insights into Mpox within the European Union. You'll discover how to recognise symptoms, adopt effective prevention strategies, and harness the power of telemedicine to access trusted healthcare, all tailored for today’s fast-moving digital world.
By the end of this guide, you'll feel empowered to protect yourself and your community. You'll also learn how modern healthcare technologies can support your well-being, wherever you are. Our goal is simple: to help you make informed decisions and take practical steps towards a healthier future.
Ready to take control of your health? Let’s dive in.
Transparency & Accuracy Commitment
This guide is based on the latest research and official guidelines from trusted organisations such as the European Centre for Disease Prevention and Control (ECDC) and the World Health Organisation (WHO).
Mpox Overview: Understanding its Presence in 2025
Once considered a rare tropical disease, Mpox (previously known as monkeypox) has firmly entered the global conversation. Since its large-scale outbreaks in 2022 and 2023, Mpox has evolved into a health concern that remains relevant for both residents and travellers within the European Union (EU) in 2025.
A Brief History of Mpox
First identified in humans in 1970 in the Democratic Republic of Congo, Mpox is caused by the monkeypox virus, a member of the orthopoxvirus family — the same family that includes smallpox.
For decades, outbreaks were largely limited to parts of Central and West Africa. However, in 2022, Mpox saw a major shift: large numbers of cases began appearing in non-endemic countries, including Europe.
Where We Are Now: Mpox in 2025
As of early 2025, Mpox has not disappeared. While major outbreaks have subsided, sporadic clusters and isolated cases still occur across Europe and globally.
Travellers, healthcare workers, and the general public must remain aware, not alarmed, but prepared.
According to the latest data from the ECDC and WHO:
- The most recent cases in Europe have involved Clade II of the virus (see the table below for differences).
- Transmission continues mainly through close physical contact.
- Public health responses now focus on rapid detection, vaccination of high-risk groups, and accessible information to prevent wider spread.
Why Mpox Awareness Still Matters
Even as new diseases emerge and the COVID-19 pandemic recedes, Mpox serves as a continuing reminder of how infectious diseases can cross borders and evolve.
Understanding Mpox helps you:
✅ Recognise symptoms early
✅ Protect vulnerable individuals (young children, immunocompromised people)
✅ Travel safely within and outside the EU
✅ Access telemedicine options if healthcare access is limited or delayed
Differentiating Clades: What It Means for You
Not all MPXV viruses are the same. In 2025, two main groups (clades) are recognised:
|
Key Aspect |
Clade I (Congo Basin) Characteristics |
Clade II (Global Outbreak) Characteristics |
|
Virulence |
Higher fatality rate (up to 10%) |
Lower fatality rate (typically <1%) |
|
Transmission |
Less efficient human-to-human; animal reservoir key |
More efficient human-to-human, especially via close contact |
|
Geographical Prevalence |
Primarily Central Africa |
Global spread, with ongoing clusters in EU |
|
Symptoms |
More severe systemic illness, larger lesions |
Often milder, sometimes atypical presentations; lesions may be fewer or localised |
Why this matters: The Clade II strain currently circulating in Europe generally causes less severe illness but can present with unusual symptoms, making public awareness and early detection essential.
Understanding Mpox: Signs, Symptoms, and Evolution
When new diseases emerge, so does a wave of misinformation. One common challenge is recognising the actual symptoms of Mpox, especially as they have evolved in recent years. In 2025, knowing what to look for — and what not to panic about — is key to protecting yourself and those around you.
Why It’s Important
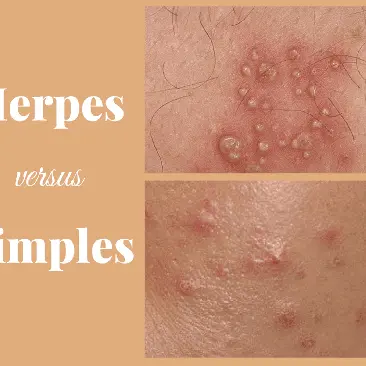
Mpox symptoms can mimic those of other common conditions such as chickenpox, herpes, or skin infections. Recent outbreaks in Europe have also demonstrated that Mpox can present with atypical symptoms, leading to cases being sometimes missed or misdiagnosed.
✅ Early detection helps you seek care faster
✅ Accurate knowledge prevents unnecessary fear and stigma
✅ Recognising subtle variations empowers you to act promptly
Common Mpox Symptoms (2025 focus: Clade II)
|
Symptom |
Description |
|
Fever |
Often the first sign, usually mild to moderate |
|
Headache |
Can accompany fever; ranges from mild to severe |
|
Muscle aches |
Common, especially in the back and limbs |
|
Fatigue |
Tiredness, sometimes significant |
|
Swollen lymph nodes |
A distinguishing feature, often in the neck, armpit, or groin |
|
Rash |
Evolves through stages: starts as flat spots, → raised bumps → fluid-filled blisters, → scabs |
|
Painful lesions |
May occur in the genital or anal areas, sometimes without a widespread rash |
|
Sore throat |
Reported in some cases, particularly in atypical presentations |
How Mpox Symptoms Differ from Similar Conditions
|
Condition |
Key Differences |
|
Chickenpox |
Rash appears more diffusely across the body, usually very itchy; no swollen lymph nodes |
|
Herpes |
Lesions are typically localised and recur in the same area; systemic symptoms (fever, fatigue) are usually milder |
|
Bacterial skin infections |
Often isolated to one area, no systemic symptoms or lymph node swelling unless severe. |
Atypical Presentations in 2025
In recent European outbreaks (Clade II), doctors have observed:
- Cases with only a few lesions, sometimes in genital or anal regions only
- Lesions appearing before other symptoms, or without fever
- Reports of rectal pain or bleeding without a visible rash
- Cases presenting with sore throat or mouth lesions first
(source: ECDC 2025 situational update)
Expert Tip
If you notice an unexplained rash, painful lesions, or flu-like symptoms — especially after close contact with someone who may have Mpox — seek medical advice early. Telemedicine can offer an initial assessment while reducing unnecessary exposure.
Preventing Mpox: Practical Steps for 2025
The good news? Mpox is preventable. While no prevention method is 100% foolproof, a few simple steps can significantly lower your risk of infection — whether at home, while travelling, or when supporting vulnerable members of your community.
How Mpox Spreads
In 2025, we know that Clade II Mpox, currently circulating in Europe, spreads mainly through:
✅ Close skin-to-skin contact, including sexual contact
✅ Contact with infectious lesions or contaminated materials (bedding, towels, clothing)
✅ Prolonged face-to-face exposure to respiratory droplets
✅ Contact with infected animals (rare in Europe but a consideration for travellers)
Practical Prevention Tips
|
Action |
Why It Matters |
|
Avoid close contact with anyone showing symptoms (rash, lesions, fever) |
The virus spreads most easily through direct contact with lesions |
|
Practise good hand hygiene (wash with soap and water or use alcohol-based hand sanitiser) |
Reduces risk from contaminated surfaces |
|
Avoid sharing personal items (towels, bedding, clothing) |
The virus can survive on materials |
|
Stay informed about outbreaks in your region or destination via ECDC or WHO updates |
Awareness helps you adjust your behaviours as needed |
|
Consider vaccination if you are in a high-risk group or if vaccination is recommended in your area |
Targeted vaccination can provide strong protection |
About Vaccination
In the EU, vaccination against Mpox is offered primarily to:
- Healthcare workers exposed to patients with Mpox
- Certain high-risk groups, including men who have sex with men with multiple partners
- Close contacts of confirmed Mpox cases
Vaccines used include the Modified Vaccinia Ankara (MVA) vaccine — a safe, non-replicating vaccine originally developed for smallpox. Studies show that it also offers good protection against Mpox (source).
Tip: If you think you might benefit from vaccination, consult your local public health service or GP.
Special Considerations for Travellers
Travelling within or outside the EU?
✅ Check current advisories for your destination
✅ Be mindful of local outbreaks
✅ Practise the same prevention steps abroad as you would at home
Preventing Mpox is about awareness, hygiene, and informed choices. A few careful actions can protect both you and those around you, helping to keep community spread under control in 2025.
The Role of Telemedicine in Mpox Care
In today’s digital age, telemedicine has become an essential tool, especially when dealing with infectious diseases like Mpox. If you suspect you may have Mpox symptoms or simply need advice, virtual consultations can offer timely support while helping to reduce the risk of spreading the virus.
Why Choose Telemedicine?
✅ Safe: You avoid unnecessary face-to-face contact, protecting yourself and others
✅ Convenient: Consult from the comfort of your home — no travel required
✅ Accessible: Many EU countries now offer public and private telehealth options
✅ Efficient: Get guidance on whether in-person testing or treatment is needed
When to Use Telemedicine for Mpox
|
Situation |
How Telemedicine Helps |
|
You have a rash or lesions and are unsure if it's Mpox |
A virtual doctor can assess your symptoms and advise next steps |
|
You’ve had close contact with someone diagnosed with Mpox |
Discuss your risk and whether you should monitor symptoms or seek testing |
|
You are self-isolating with mild Mpox symptoms |
Access follow-up care and advice without leaving home |
|
You need vaccination advice |
Learn whether vaccination is recommended for you and where to obtain it |
How to Access Telemedicine Services in the EU
Many EU countries now support public health teleconsultations, and private providers also offer rapid appointments:
- Public health services (NHS in the UK, Assurance Maladie in France, Krankenkassen in Germany, etc.) often provide free or low-cost telehealth options
- Private telemedicine platforms can supplement public services if you want quicker access.
Always use verified, reputable platforms. Your national health authority website will often list trusted telehealth providers.
A Word of Caution
While telemedicine is excellent for initial assessment and follow-up, in-person medical care is essential if you:
- Experience severe symptoms (high fever, difficulty breathing, severe pain)
- Develop complications
- Need laboratory testing or hospital-based treatment.
In these cases, your telemedicine provider can help guide you to the appropriate next steps.
Expert Tip: If you’re unsure whether to use telemedicine or visit a clinic, start with a virtual consultation — it’s a low-risk first step that can save time and reduce anxiety.
Conclusion & Key Takeaways
As we move through 2025, Mpox remains a health concern, but one that you can manage confidently with the right information and support.
Here’s what we’ve covered:
- Mpox is still present in Europe, with Clade II causing milder, but sometimes atypical, infections
- Recognising symptoms early and knowing how they differ from similar illnesses is key
- Prevention starts with awareness, hygiene, and vaccination, where recommended
- Telemedicine plays a vital role in helping you access advice and care safely and conveniently
In this evolving health landscape, staying informed empowers you to protect yourself, your loved ones, and your community.
How Mobi Doctor Can Help
If you suspect Mpox exposure, notice symptoms, or simply want trusted medical guidance, Mobi Doctor offers quick, secure access to qualified doctors — all from the comfort of your home.
- No waiting rooms
- Discreet, private consultations
- Guidance on next steps, testing, and treatment
- Support for managing symptoms and accessing vaccines where available
Tip: Early action makes a difference. If in doubt, don’t wait — reach out to a trusted telemedicine service like Mobi Doctor for personalised advice.
Final Thought
Knowledge is your best defence. By understanding how Mpox is evolving and how to access modern healthcare solutions, you’re already taking an essential step towards a healthier 2025.
Stay informed. Stay protected. Stay connected to care.