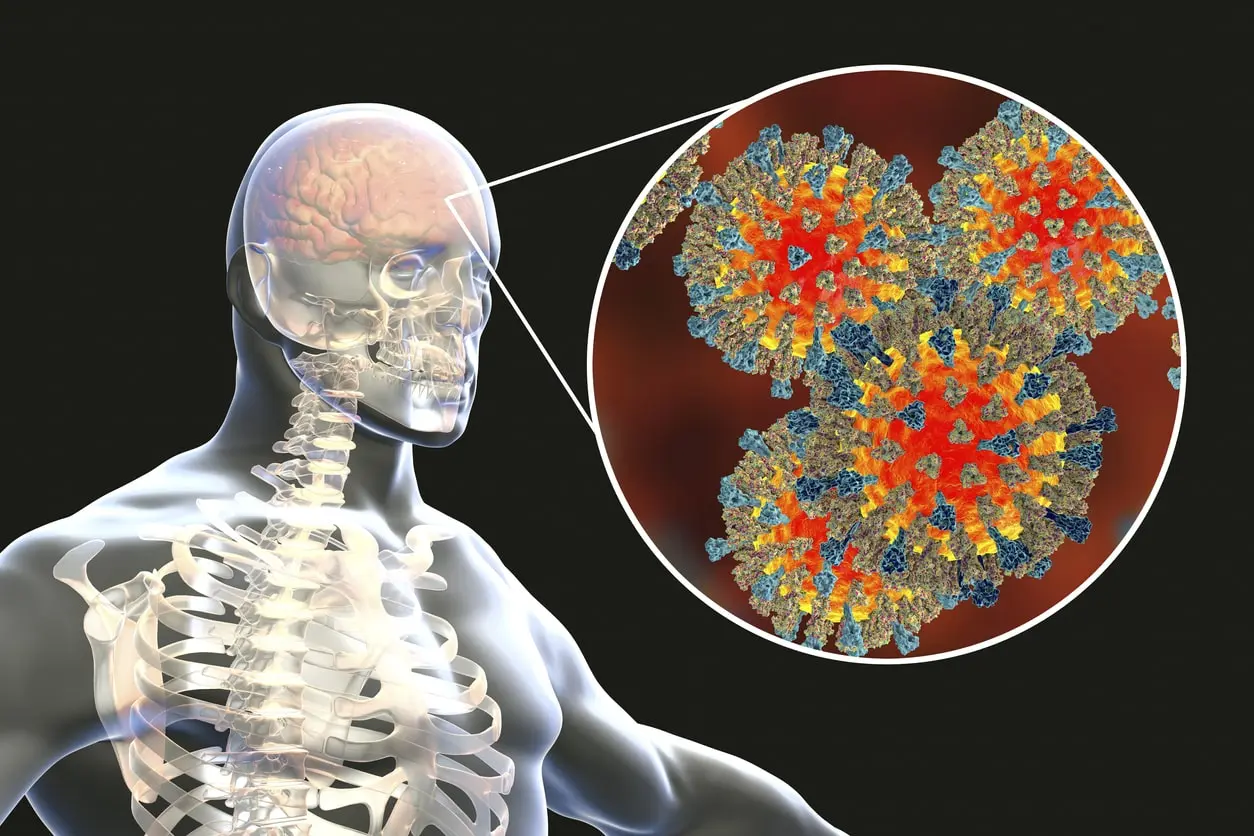
Low Serotonin And Gut Inflammation May Cause Brain Fog In Long COVID.
A significant percentage of individuals who contract SARS-CoV-2, the virus responsible for COVID-19, suffer from the after-effects of the disease, known as Long COVID.
A variety of neurocognitive and psychiatric effects have been identified, with more than 200 symptoms in total.
Researchers have demonstrated that individuals infected with SARS-CoV-2 have decreased levels of serotonin in their bodies for up to 3–22 months post-infection.
The discovery suggests that clinical studies monitor serotonin levels to determine whether a patient has long COVID-19.
Approximately 5-10% of individuals who have had a SARS-CoV-2 infection will suffer from long COVID or post-COVID-19 syndrome. Those hospitalised with the virus have a higher risk of developing this syndrome, while those vaccinated have a lower risk.
Since 2020, when the first people suffering from the long-term effects of COVID-19 began sharing their stories, more than 200 symptoms can be caused by the virus, including those affecting the brain, such as fatigue, difficulty concentrating, memory loss, and "brain fog".
From early 2021, some experts started to use the phrase “neuro COVID” to refer to the signs and symptoms experienced by those suffering from COVID-19 for more than three months after their initial infection.
Even though post-viral syndromes have not been extensively studied before the pandemic, it remains unclear what causes this symptom.
Before the pandemic, little effort had been devoted to researching post-viral illnesses. This has resulted in a lack of understanding of the neurological abnormalities in those who have had the flu or contracted COVID-19.
Serotonin May Play A Role In Long COVID Brain Fog.
The COVID-19 pandemic has shifted focus as researchers have attempted to uncover the underlying cause of long COVID-19 cases. They have been looking for biomarkers that could be used in diagnostics and treatments to understand this prolonged illness better.
Evidence is beginning to point to a link between inflammation, microglial activation, and neurocognitive symptoms in those infected with COVID-19 for a prolonged period.
Research revealed that individuals with long-term COVID-19 symptoms have decreased serotonin levels. Months after infection, SARS-CoV-2 viral RNA stored in the intestines mediated an inflammation pathway.
Combining data from prior research, the study's authors examined the biochemical composition of various groups of people who had experienced symptoms of long COVID-19 for a period ranging from three to twenty-two months since they were confirmed to be infected with SARS-CoV-2.
To better understand the symptoms of COVID-19, researchers split 58 patients into 8 clusters based on their symptoms. To compare the clusters, the scientists examined the biochemical profiles of the 58 patients. They compared them to the biochemical profiles of those infected with SARS-CoV-2 and those who had recovered from the virus with no remaining symptoms.
Findings from the study showed that some individuals with prolonged COVID still had evidence of the virus in their faecal samples many months following infection, indicating that the virus had stayed in the digestive system.
Lower serotonin levels four months after active SARS-CoV-2 infection were found to correlate with the number of symptoms experienced by those with long COVID.
However, serotonin levels during the active infection did not indicate a person’s risk of developing long COVID.
A New Biomarker For Long COVID?
Subsequent studies with mice revealed that the immune response to the residual viruses triggered inflammation that impeded the uptake of tryptophan - an essential component of serotonin - in the gut of the mice and reduced their serotonin storage.
Serotonin is a neurotransmitter that plays a vital role in the body. It regulates mood, sleep, digestion, nausea, healing, blood clotting, and sexual desire. It also enables communication between nerve cells by sending signals between them.
Scientists proposed that as there is less signalling in the hippocampus, a brain area associated with memory formation, in individuals with prolonged COVID-19, memory impairment in mice may result from decreased serotonin signalling in the hippocampus.
Researchers examined the serotonin levels in the brain and found that they were within normal range. However, they also observed that the communication between nerves outside the brain, such as the vagus nerve, was impaired, resulting in decreased memory function.
Low serotonin levels could potentially be used to identify those with prolonged symptoms of COVID-19.
According to research, potential biomarkers for long-term COVID-19 diagnosis and treatment include viral components detected in stool samples and decreased serotonin levels in the blood.
Could Antidepressants Treat Long COVID Brain Fog?
Researchers have discovered that patients with Dengue fever tend to have lower serotonin levels, suggesting that the same concept could be applied to other medical conditions.
Researchers have found that some of the processes behind long COVID are not exclusive to this condition but can also be seen in other post-viral syndromes.
Due to the potential of long COVID research discoveries, individuals affected by other post-viral syndromes could benefit from the progress.
Symptoms of Long COVID may be comparable to those observed in other illnesses with chronic symptoms, such as influenza. Further research is necessary to determine if the proposed connection between viral reservoirs, prolonged inflammation, decreased serotonin levels, vagus nerve issues, and neurocognitive issues is linked to post-flu symptoms.
‘Meritorious’ Research On Long COVID
The researcher noted that COVID-19 is a complex condition, and its cognitive and emotional issues could have various causes. He stated that the research is commendable in its attempt to comprehend these effects.
Based on the data, there is a strong argument for conducting clinical trials to determine if SSRIs can improve cognitive functioning in individuals with prolonged COVID-19 infection and 'brain fog', the name commonly associated with cognitive impairments seen in those with long-term COVID-19.
You can connect with one of our doctors at Mobi Doctor with the click of a button and get the care you need.