How Eczema Can Create Adverse Mental Health Symptoms
- Eczema, or atopic dermatitis, affects approximately 3% of adults worldwide.
- The persistent itchiness and visible symptoms of eczema can harm an individual's overall well-being and psychological state, significantly affecting their quality of life.
- A significant majority of individuals with eczema, approximately 72%, experience negative mental health symptoms for up to 10 days per month. Furthermore, a notable 17% of individuals with eczema endure these symptoms for more than 11 days each month.
Eczema, also known as atopic dermatitis, affects 3% of the global adult population, making it a prevalent skin condition worldwide.
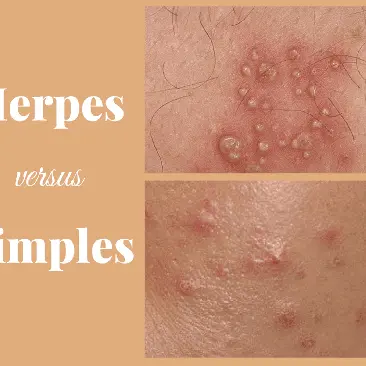
Eczema is a long-lasting skin condition characterised by inflammation, resulting in excessively dry, coarse, and irritated skin that often becomes itchy.
While there is no known cure for eczema, several treatments can alleviate symptoms and improve the overall quality of life. Various treatments can be used, including topical creams, oral medications, changes in lifestyle, and avoiding triggers that can exacerbate the symptoms.
Research has consistently demonstrated a strong link between atopic dermatitis and its detrimental effects on an individual's mental well-being and overall psychological state.
According to a recent study conducted by the National Eczema Association, it was found that 72% of individuals with eczema experience negative mental health symptoms for a period ranging from one to 10 days per month. Furthermore, 17% of those surveyed reported experiencing these symptoms for more than 11 days per month.
Is There A Relationship Between Eczema And Mental Health?
Recognising the established link between atopic dermatitis and mental health problems, the researchers opted to undertake a study aimed at gauging the psychological well-being of individuals with eczema.
In January 2020, a study published that adults who have eczema are at a higher risk of developing new diagnoses of depression and anxiety. Furthermore, the severity of eczema was found to be directly linked to the prevalence of depression.
Furthermore, the study published in March 2021 revealed a notable correlation between atopic dermatitis and an increased prevalence of depression, with a significantly higher number of individuals with skin conditions reporting depressive symptoms compared to those without.
An Unmet Need For Addressing Mental Health Concerns
The researchers conducted an online survey and received responses from 954 adults diagnosed with atopic dermatitis.
Out of the individuals surveyed, it was found that 23% sought treatment for their eczema from an allergist. At the same time, 124 respondents relied on their primary care provider, who may not specialise in eczema treatment, as their allergist.
According to survey data, a significant majority of respondents, precisely 72%, reported experiencing adverse mental health symptoms for up to 10 days within a month. Additionally, 17% of participants reported suffering from adverse mental health for more than 11 days.
The high prevalence of atopic dermatitis and its correlation with adverse mental health outcomes should not be overlooked. Extensive research has consistently demonstrated the vital link between atopic dermatitis, particularly in cases of moderate to severe severity, and the detrimental impact on mental well-being.
The current approach to addressing mental health concerns among atopic dermatitis patients falls short of meeting their needs.
The Need For Eczema Holistic Care
The online survey shows that a significant portion of respondents (35%) had refrained from discussing their mental health concerns with their allergist. A more substantial majority (57%) reported that their allergist had never inquired about their mental well-being.
The focus on addressing skin symptoms is crucial, but it fails to address other significant concerns that patients may have. By recognising the influence of atopic co-morbidities on mental health, allergists have the potential to alleviate emotional burdens associated with atopic dermatitis. To improve the standard of care, allergists must engage in open discussions about mental health with patients, extending beyond the impact on their skin. Additionally, allergists should be aware of and willing to refer patients to mental health resources and other healthcare professionals who can provide further assistance.
However, this approach may not be adequate for some patients who require a more thorough assessment. Additionally, this approach may be inadequate for identifying underlying issues that may be causing the patient's mental health issues.
The focused mental health evaluation instruments provide a more comprehensive picture of the individual's mental health, while the sub-elements of other patient-reported outcomes instruments, such as the ADCT, provide more detailed insight into the individual's condition. The focused instruments provide a more comprehensive overview of mental health, while the sub-elements give a more detailed view of specific aspects of the individual's condition.
How Eczema Affects Mental Health
The sensation of itching, transmitted by the same nerve fibres as pain, can be highly disruptive for people with skin conditions such as atopic dermatitis. This can cause significant discomfort and disturbance throughout the day and during sleep.
The nighttime exacerbation of itch can disrupt sleep, leading to emotional dysregulation and an increased risk of depression. Furthermore, individuals experiencing depression often struggle with sleep disturbances, including a reduction in the amount of rejuvenating slow-wave sleep obtained each night.
This study further emphasises the perpetuating cycle in which patients with this condition are trapped. It can also lead to other skin problems, such as acne and eczema. Reducing stress can help to manage atopic dermatitis symptoms and prevent flares.
Healthcare providers are now taking a holistic approach to patient care by inquiring about their physical and mental well-being.
The findings of this study play a significant role in shaping and guiding the ongoing discourse.
The availability of specific data allows us to present evidence-backed arguments and have more informed discussions about mental health with our patients.
Although several studies have suggested a link between eczema and anxiety and depression, the existing data remains inconclusive.
Further research is essential to comprehensively explore the wide-ranging effects on individuals' happiness and satisfaction with life.
Connect with one of our doctors at Mobi Doctor with the click of a button and receive the care you require.